Limb apraxia in the cortico-basal syndrome
1 - Introduction
Cortico-Basal Degeneration (CBD: Cortico-Basal Degeneration), or Rebeiz
syndrome, was first discovered in 1968 by Rebeiz, Kolodny, and Richardson. During the
clinical examination of three adult patients, the researchers identified the presence of a
neurological pathology characterized by deficits in muscle movements, involuntary motor
activities and initially preserved mental faculties. Post-mortem examination led to the
discovery of a new disease that the researchers called "corticodentatonigral degeneration
with neuronal achromatism" (Rebeiz et al., 1968).
CBD is part of a group of diseases called "Parkinsonisms Plus", defined in this way because
they present signs and symptoms that recall Parkinson's disease, from which they take their
name. CBD is a very rare neurodegenerative disease, affecting only 1% of patients clinically
diagnosed with parkinsonism (Stamenova et al., 2009). It is an asymmetric, akinetic-rigid
syndrome, characterized by progressive degeneration of some areas of the brain, in
particular the frontal, parietal and basal ganglia (Dickson et al., 2002).
1.1 - Limb apraxia: brief introduction and interpretative models
Motor disturbances have been found to be the first to be observed in patients with CBS (CBS:
Cortico-Basal Syndrome) and among these the most common is ideomotor apraxia, or limb
apraxia
(Graham et al., 2003).
Limb apraxia is one of the most recognized types of apraxia and, although it is defined as
the inability to perform specialized movements, it is not caused by sensorimotor or
comprehension deficits. It usually occurs as a result of left parietal lesions, although it
can often occur as a result of extrapyramidal lesions.
Apraxia was first observed by John Hughlings Jackson, in 1861, in patients with aphasia, who
showed an inability to perform simple limb movements (Pearce JM, 2009). However, he did not
give this disorder the name by which it is still recognized.
To date, there are various interpretative models that explain the behavior of this
phenomenon and its evolution, hypothesizing the internal structures involved in the
behavioral manifestation of this disorder. In the Figure 1 are specified the
main interpretative models developed from 1900 to the one developed by Buxbaum.
Geschwind later defined limb apraxia as a disconnection syndrome between motor areas and
conceptual areas. This disconnection, which involved in particular the supramarginal gyrus,
which is located between the Wernicke area and the frontal cortex, would be the cause of an
impairment in the execution of movements (Geschwind, 1965).
In 1982, De Renzi and Faglioni suggested a model in which the Praxic center was located in the
left parietal lobe, which was connected to the left premotor cortex. According to this model,
apraxia would be caused by a disconnection between the areas that process the information and
the areas where the movement is programmed (De Renzi et al., 1982).
Heilman and colleagues, in 1997, proposed the existence of two components within the model of
practice: one of execution and production (earlier) and the other conceptual-representative
(later). According to this model, the representation of the action is stored in the left
inferior parietal lobe; to perform a movement, the signal is sent to the premotor cortex, which
is located in the frontal (anterior) lobe. According to Heilman and Rothi, therefore, damage to
the anterior areas would cause a deficit in the execution and production components of the
movements (Heilman et al., 1997).
Finally, Buxbaum (2001) proposed a model of practice in which representations of actions are
stored in the inferior parietal lobe. Consequently, damage to this area would result in impaired
recognition and production of specialized actions (Buxbaum, 2001).
2 - Corticobasal syndrome and presentation of limb apraxia
2.1 - Clinical features
The classic clinical presentation of CBD is characterized by a progressive asymmetric motor dysfunction, which presents symptoms such as rigidity, myoclonia and the phenomenon of the alien hand, initially in a specific limb. Later, the disease also extends to other limbs and can affect gait and cognitive function (Armstrong R.A., 2016).
2.1.1 - Extrapyramidal characteristics
The extrapyramidal characteristics of CBD emerge from the onset of the disease and are the most common manifestations recorded in patients. They include some motor functions including Parkinsonism, dystonia and myoclonia.
2.1.2 - Cortical characteristics
In addition to the extrapyramidal features described above, some cortical signs are also commonly observed in CBD, among which the most important are: limb apraxia, alien hand phenomenon and cortical sensory loss.
Limb apraxia
Apraxia is one of the main symptoms of CBD, included in all the diagnostic
criteria developed so far. There are several types of apraxia, however, ideomotor apraxia is
the most described form of apraxia in CBD and is characterized by the inability to perform a
movement when prompted on verbal command or performed on imitation.
From an analysis of the frequency of cortical features in CBD patients observed in brain
banks and in studies presenting a sample of at least 5 cases presenting CBD, performed by
Armstrong et al. (2013), it was concluded that 46/102 (45%) of cases have limb apraxia since
the onset of the disease; while in 81/142 (57%) limb apraxia was diagnosed during the
progression of the disease.
Evaluating the presence of limb apraxia in patients with CBD is particularly difficult,
especially if the subjects have already developed other typical motor manifestations of CBD,
such as limb stiffness, dystonia, and myoclonia. Certainly, a systematic assessment of
apraxia can facilitate the differential diagnosis between patients with CBS or other similar
clinical syndromes.
2.2 - Diagnostic criteria
Several sets of diagnostic criteria have been proposed over the years, all
of which focus primarily on the phenotypic spectrum of CBD. Among all, the most recognized
are: the criteria of Lang et al. (1994), Boeve et al. (2003) and those of Bak and Hodges
(2009).
These sets of criteria have some characteristics in common. Indeed, all three agree that
CBS, i.e. the classic clinical presentation of CBD, is characterized by the presence of
cortical dysfunction, such as ideomotor apraxia, alien limb phenomenon, cortical or sensory
loss, and extrapyramidal dysfunction, such as stiffness, myoclonia or dystonia. Despite
this, none of the three criteria specify at which stage of the disease these characteristics
should present themselves.
However, the three criteria also have some differences between them and due to the various
discrepancies between the methods of diagnosing CBS, it is difficult to determine which of
these criteria is the most valid and reliable in diagnosing CBS.
2.2.1 - Armstrong's criteria
In 2013, Armstrong et al. introduced a new diagnostic criterion, based on a
careful critical analysis of the literature of CBD clinical pathological studies and on the
collection of original data from brain banks, which collects all the different phenotypes
and various clinical syndromes that CBD can present.
This review also suggested that CBD may also be associated with other clinical syndromes
other than classic CBS. From an examination of 210 cases of CBD, collected from the
literature, 4 clinical phenotypes associated with this pathology emerged (Armstrong et al.,
2013):
- CBS (probable and possible);
- FBS (Frontal Behavioral-spatial Syndrome): frontal spatial behavioral syndrome;
- naPPA (Nonfluent / Agrammatic variant of Primary Progressive Aphasia): non-fluid / agrammatic variant of primary progressive aphasia;
- PSPS (Progressive Supranuclear Palsy Syndrome): syndrome of progressive supranuclear palsy.
4 - Impairments in motor tasks in patients with cortico-basal syndrome
CBS is, in short, a movement disorder that results from a lesion of
cortical and subcortical areas. Specifically, a particular type of voluntary movement
disorder, namely limb apraxia, is included in the diagnosis criteria for CBS.
Limb apraxia is characterized by the inability to imitate gestures and / or perform
pantomimes; the latter consists in the mimic demonstration of the use of an object or of a
sequence of actions with an object.
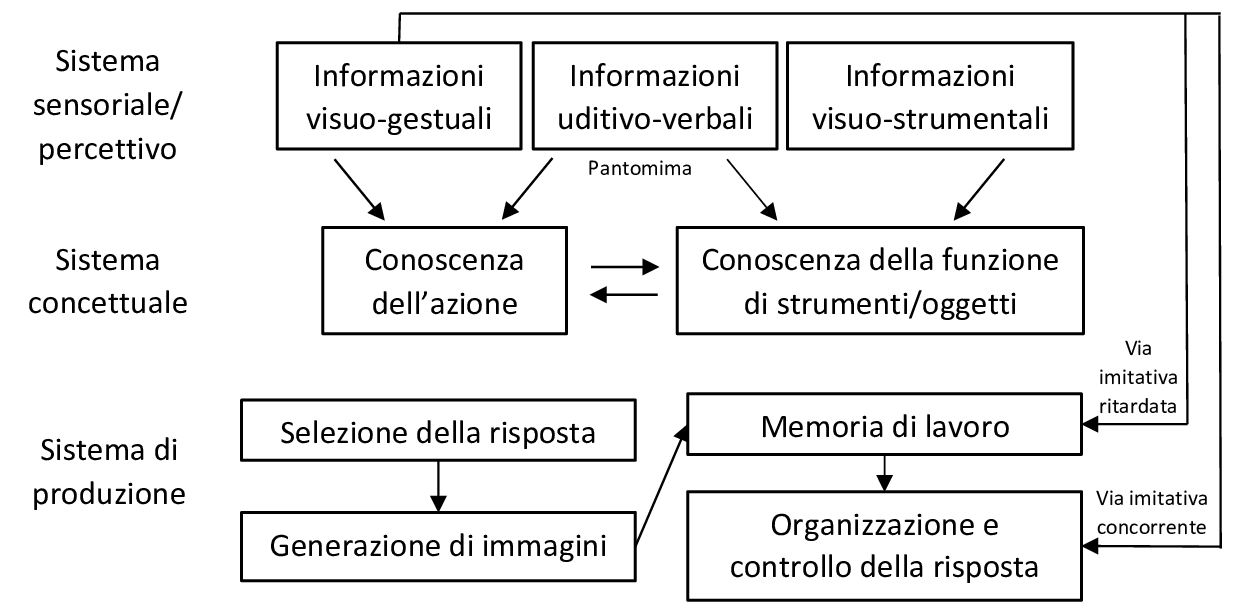
Injury to one of these pathways results in a specific pattern of praxis deficit. It is therefore
necessary to perform a thorough evaluation of the various gestural performances in different
modalities and for multiple types of gestures, in order to be able to determine which particular
system of practice has been affected.
Since CBS is a progressive neurodegenerative disease, over time it tends to also affect
cognitive functions and, consequently, decreases the ability of patients to understand and be
able to perform complex tasks. It is therefore important to evaluate patients in praxic tasks,
as well as in cognitive and neuropsychological tests, at the onset of the disease.
5 - Conclusion
Limb apraxia is evident in the production and execution of specific limb
movements and is usually present early in the onset of CBS: a progressive neurodegenerative
parkinsonian disease characterized by motor system dysfunction and multiple cognitive
deficits.
Although limb apraxia initially manifests in only one limb, the disorder can expand over
time to involve others. This worsening of apraxia is caused by the progression of CBS, which
over time extends and damages other brain areas, in addition to the fronto-parietal ones.
CBS and limb apraxia share the same neuroanatomical correlates: at the cortical level,
lesions occur mainly in the frontal and parietal areas, while at the subcortical level,
dysfunctions of the white matter and basal ganglia can be observed.
It is important to recognize the initial symptoms of limb apraxia in CBS before CBS
progresses, so that appropriate and managed treatment can be given to the patient in a
multidisciplinary rehabilitation setting. For this reason, it is necessary to perform an
analysis of the praxis components in a detailed clinical examination, examining the patient
in the various modes and types of gestures described above. In order to understand which
systems of the practice model are damaged and which intervention is most effective for the
individual patient, it is useful to take note of the type and quantity of errors made by the
patient in the evaluation phase.
